Evaluation and comparison of the new swept source
OCT-based IOLMaster 700 with the IOLMaster 500
ABSTRACT
Purpose To compare the measurements and failure rates obtained with a new swept source optical coherence tomography (OCT)-based biometry to IOLMaster 500. Setting Eye Clinic, Baskent University Faculty of Medicine, Ankara, Turkey.
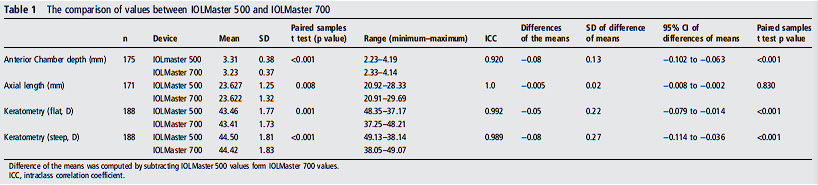
Design Observational cross-sectional study and evaluation of a new diagnostic technology. Methods 188 eyes of 101 subjects were included in the study. Measurements of axial length (AL), anterior chamber depth (ACD), corneal power (K1 and K2) and the measurement failure rate with the new Zeiss IOLMaster 700 were compared with those obtained with the IOLMaster 500. The results were evaluated using Bland–Altman analyses. The differences between both methods were assessed using the paired samples t test, and their correlation was evaluated by intraclass correlation coefficient (ICC). Results The mean age was 68.32±12.71 years and the male/female ratio was 29/72. The agreements between two devices were outstanding regarding AL (ICC=1.0), ACD (ICC=0.920), K1 (ICC=0.992) and K2 (ICC=0.989) values. IOLMaster 700 was able to measure ACD AL, K1 and K2 in all eyes within highquality SD limits of the manufacturer. IOLMaster 500 was able to measure ACD in 175 eyes, whereas measurements were not possible in the remaining 13 eyes. AL measurements were not possible for 17 eyes with IOLMaster 500. Nine of these eyes had posterior subcapsular cataracts and eight had dense nuclear cataracts. Conclusions Although the agreement between the two devices was excellent, the IOLMaster 700 was more effective in obtaining biometric measurements in eyes with posterior subcapsular and dense nuclear cataracts.
INTRODUCTION
The advancement of new technologies in intraocular lens (IOL) design and surgical techniques has increased the expectations of patients for exceptional postoperative vision without any refractive correction. The correct measurement of axial length (AL) and corneal power are crucial for the calculation of IOL power and achievement of the desired postoperative refraction.1 Modern optical biometry devices use either partial coherence interferometry (PCI) or optical low coherence reflectometry (OLCR) to measure several variables including AL. In addition they can measure keratometry (K), anterior chamber depth (ACD), lens thickness (LT) and horizontal white-to-white (WTW) corneal diameter using different approaches.2 Moreover, the built-in software in these devices provides more accurate IOL power calculation and multiple choices of IOL formulas.3 The IOLMaster (Carl Zeiss Meditec AG, Jena, Germany) is the gold standard of modern optical biometry devices. It uses the principle of PCI to obtain AL with high precision.4 5 Several reports have shown the accuracy of IOLMaster (IOLMaster or IOLMaster 500) for IOL calculation in routine and complicated cataract cases.6–9 However, measurements can be difficult or unreliable with corneal opacities, macular diseases, advanced and posterior subcapsular (PSC) cataracts, vitrectomised eyes or poor fixation for PCI or OLCR based devices.10 11 The IOLMaster 700 (Carl Zeiss Meditec AG, Jena, Germany), which is the first swept source optical coherence tomography (OCT) based biometry, was introduced recently. It enables OCT imaging and visualisation across the entire length of the eye. It provides an image-based measurement, allowing the surgeon to view the complete longitudinal section of the eye. Therefore, it may identify irregular eye geometries, such as lens tilt. Additionally, imaging of the fovea may alert the
observer to insufficient fixation during measurements. It also uses telecentric keratometry for corneal power measurements, similar to the IOLMaster 500. Briefly, it was introduced as an advantageous diagnostic device in an attempt to improve refractive results after cataract surgery. The purpose of this study was to compare the agreement between IOLMaster 500 and IOLMaster 700 values for ACD, AL and keratometry. Measurement failure rates with both devices were also recorded and compared.
PATIENTS AND METHODS
This observational cross-sectional study comprising patients with cataract was performed at the Başkent University Faculty of Medicine, Department of Ophthalmology, Ankara, Turkey. The study was performed according to the Declaration of Helsinki. The University’s ethics committee approved the study design and protocol. The patients were fully informed about the purpose of the study, after which they provided informed consent. Patients who were either diagnosed for the first time or who were under follow-up for cataract were included in the study. Patients were recruited during a 3-month period between April and June 2015. All patients were examined by the same physician (AA) and in addition to routine ophthalmological examinations, cataract types were recorded as nuclear, cortical or PSC according to Lens Opacities Classification III scoring system (LOCS III).12 Biometric measurements were performed before pupillary dilatation in all patients. Patients who were unable to cooperate and fixate adequately during the measurements, with advanced macular problems like cystoid macular oedema or elevated scars, additionally whom had previous ocular surgery and irregular corneal surfaces were not included in the study. Corneal surface was investigated by Scheimpflug system (WaveLight Allegro Oculyzer; WaveLight AG, Erlangen, Germany). AL, ACD and corneal power (K1 (flattest axis); K2 (steepest axis of corneal curvature 90° apartfrom flat axis)), and failure rates for both instruments were compared.
Instruments
IOLMaster 500 uses the PCI principle for AL measurements, a six-point telecentric technique for K readings and an imagebased slit lamp system for ACD measurements. It can also measure WTW distance. However, LT and central corneal thickness (CCT) measurements are not available on IOLMaster 500. With this device, five consecutive measurements of AL and ACD, and three consecutive keratometry measurements were performed. A signal to noise ratio (SNR) value for AL readings is calculated. The manufacturer does not recommend the use of the measurements with SNR value less than two. Quality of keratometry testing can be verified by visually checking the quality of the readings.
IOLMaster 700 automatically takes swept source OCT scans
and measures AL, along with CCT, ACD and LT. AL measurements are the average values of three scans in each of six meridians. For K readings, three average Ks, each of five single measurements are taken and the final average K readings are calculated. On the IOLMaster 700, the operator can see the whole scan image and visually check the eye geometry and axis of the measurements; also the foveal scan checks the correct fixation by the patient. SD values of the ACD, LT and AL measurements are calculated and the device warns the operator of low-quality results if the SD for ACD >0.021 mm, for LT >0.038 mm and for AL >0.027 mm. Biometry measurement technique Biometric measurements were performed using IOLMaster 500 and IOLMaster 700 consecutively by the same technician for the first 100 eyes and the order was reversed for the remaining eyes. The quality control criteria for both devices were used in accordance with the above-mentioned manufacturer recommendations. If measurements were not possible in accordance with limits, they were recorded as measurement failures for either device. The same examiner, who was trained according to the
manufacturer’s recommendations, performed all tests. All IOLMaster 700 scans were checked by the same surgeon (AA) for foveal scans to ensure the correct axis measurements and the scan was repeated if the patient was not fixating correctly.
Statistical analysis
The required sample size was calculated using the following formula: n=[(2×tf,0,95×SD)/CI]2 with tn–1;1–α/2=1, 7 (quantile of t distribution for expected sample size n>50 and α=0.05; SD; CI).2 The anticipated SDs were based on the results from preliminary study data for initial power analysis.13 The results were evaluated using intraclass correlation coefficients (ICCs), Bland–Altman plots and paired samples t tests. Left and right eyes were included in the subsequent analysis, as most of the variation in the ocular variables considered in this study is found within rather than between the left and right eyes